School is back in session!
As a parent, we’re sure you’re excited that the summer chaos, coordinating camps and activities, and simply having your children around 24/7 have ended!
As you know, going back to school typically means your child gets sick more frequently. So, how can you safeguard your child and the rest of your family’s wellness this back-to-school season?
Below are a few tips.
Stay Up-to-Date on Immunizations and Vaccines
Vaccination requirements typically vary on a state-by-state basis or even in a school-specific district. To find out precisely what immunizations your child needs, contact your local school board.
The Centers for Disease Control and Prevention’s (CDC’s) Advisory Committee on Immunization Practices, the American Academy of Pediatrics, and the American Academy of Family Physicians recommend a few specific vaccines based on your child’s age. These are as follows:
By Age Two
A vaccination series of the following vaccines should be completed in all children by age two:
- Hepatitis B
- DTaP (diphtheria, tetanus, and pertussis)
- Hib (Haemophilus influenzae)
- Polio
- Pneumococcus
- MMR (measles, mumps, rubella)
- Varicella (protects against chicken pox)
In addition, annual flu vaccines are recommended for infants from six to 24 months, as this age group is at high risk of complications from contracting the flu.
Hepatitis A vaccines may also be recommended starting at age 2 for those in high-risk groups or areas.
Age Four to Six
Typically, boosters are recommended between ages four to six for DTaP, Polio, and MMR. Those who are younger than nine and have not received the flu vaccine, need two doses of the vaccine given more than one month apart. After age nine, annual vaccination is recommended.
Children with asthma or lung diseases, sickle cell anemia, HIV, diabetes, and heart or kidney disease should receive the influenza vaccination annually.
Age 11 to 12
At around age 11 to 12, a pediatrician visit is recommended to review vaccinations and ensure all necessary immunizations have been provided. At this age, a hepatitis B, MMR, or varicella vaccine may be given if missed or incomplete at earlier ages.
Your child may also receive a combination of boosters for tetanus and diphtheria (if five years have passed since the last Td vaccine). Children with a high risk of complications from the flu should receive an annual vaccine.
Attend Annual Checkups
Annual doctor’s office visits and check-ups can help prevent greater health issues later on down the line. These check-ups can help identify hearing and vision issues, malnutrition, and other lifestyle imbalances.
Hearing and Vision Issues
Vision and hearing losses are often overlooked in children at a younger age. These issues are difficult to identify if your child is not getting tested in their annual check-up for vision and hearing ability.
Identifying these issues early on can make a huge impact on your child’s ability to learn and engage both in school and at home.
Malnutrition
A child’s development depends on proper nutrition, both physically and cognitively. Malnutrition is an issue that impacts children globally, including in the U.S.
Annual checks and doctor’s visits can help give you greater insight into how your child is developing compared to other children of the same age. A slight change in nutrition can have a huge impact on your child’s ability to learn.

MEC Covered Services for Children
To make sure your child can receive the care they need to remain healthy during the school year, you need proper insurance coverage.
Minimum essential coverage (MEC) offers an affordable coverage option to keep you and your family healthy at all times.
Some of the services covered for children include:
- Alcohol and drug use assessments for adolescents
- Autism screening for children at 18 and 24 months
- Behavioral assessments for children at 0 to 11 months, one to four years, five to 10 years, 11 to 14 years, and 15 to 17 years
- Bilirubin concentration screening for newborns
- Blood Pressure screening for children at 0-11 months, one to four years, five to 10 years, 11 to 14 years, and 15 to 17 years
- Blood screening for newborns
- Cervical dysplasia screening for sexually active females
- Depression screening for adolescents
- Developmental screening for children under age three
- Dyslipidemia screening for children at higher risk of lipid disorders at one to four years, five to 10 years, 11 to 14 years, and 15 to 17 years
- Fluoride chemoprevention supplements for children without fluoride in their water source
- Fluoride varnish for all infants and children as soon as teeth are present
- Gonorrhea preventive medication for the eyes of all newborns
- Hearing screen for all newborns; and for children once between 11 and 14 years, 15 and 17 years, and 18 and 21 years
- Height, weight, and body mass index measurements for children at 0 to 11 months, one to four years, five to 10 years, 11 to 14 years, and 15 to 17 years of age
- Hematocrit or hemoglobin screening for all children
- Hemoglobinopathies or sickle cell screening for newborns
- Hepatitis B screening for adolescents ages 11 to 17 years at high risk.
- HIV screening for adolescents at higher risk
- Hypothyroidism screening for newborns
These services in combination with preventative measures taken at home can help keep your family and your children safe during the back-to-school influx of sickness.
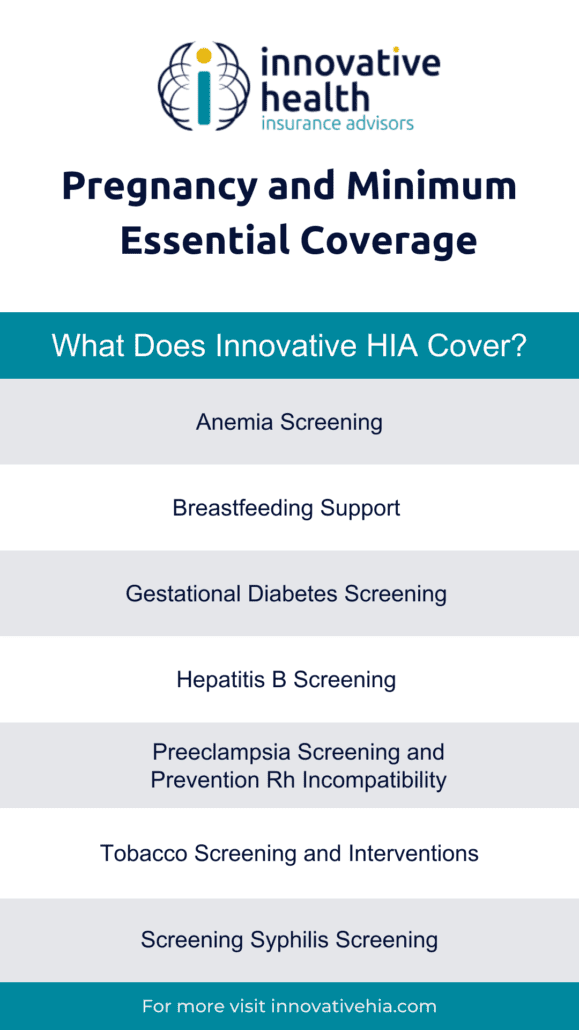
Looking to start a family or grow your current family? Take a look at one of our recent articles to learn about pregnancy and minimum essential coverage.