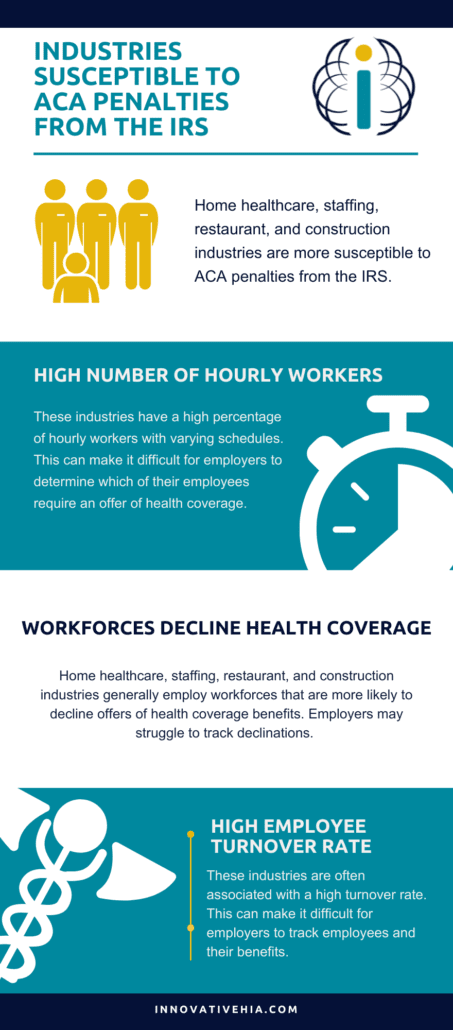
While all organizations are susceptible to receiving IRS penalties, some industries are particularly vulnerable. These industries include home healthcare, staffing, restaurant, and construction industries.
Why are these industries under fire from the IRS? Let’s take a look.
These Industries Typically Have a High Number of Hourly Workers
Home healthcare, staffing, restaurant, and construction industries have a high percentage of hourly workers with varying schedules. This can make it difficult for employers to determine which employees are ACA full-time and require an offer of health coverage.
HR is often a non-centralized function, making it challenging to gather the data necessary for compliance.
High Staff Turnover Rates
These industries are often associated with a high employee turnover rate. This can make it difficult for employers to track employees as their benefits.
Workforces that Disproportionately Decline Health Coverage
Home healthcare, staffing, restaurant, and construction industries generally employ workforces that are more likely to decline offers of health coverage benefits. Employers may struggle to track declinations and face ACA penalties from the IRS.
How Can Organizations Ensure They Are Complying with ACA Requirements?
Employers can ensure they are ACA compliant by determining the accurate full-time and part-time status of employees under ACA. Employers may experience significant ramifications for misclassifying employees.
Additionally, employers should familiarize themselves with their requirements under the ACA’s Employer Mandate. For example, employers with 50 or more full-time employees, or ALEs, must:
- “Offer Minimum Essential Coverage (MEC) to at least 95% of their full-time employees (and their dependents) whereby such coverage meets Minimum Value (MV); and
- Ensure that the coverage for the full-time employee is affordable based on one of the IRS-approved methods for calculating affordability.”
For more information, read on for the full article from the ACA Times.
These Industries are Most at Risk for ACA Penalties From the IRS
The home healthcare, staffing, restaurant, and construction industries are under fire from the IRS for failing to comply with the ACA. Organizations within these industries have been shocked to receive ACA penalty notices from the IRS that are in the millions of dollars.
Of course, all types of organizations – hospitality, manufacturing municipal governments, non-profits, and other industries – are receiving IRS penalty notices too. However, the four industries mentioned above seem to be getting more than their fair share.
Here’s why these industries are so susceptible to receiving ACA penalties:
- HR is often a non-centralized function, making it challenging to gather the data necessary for compliance
- They have a high percentage of hourly workers with varying schedules, making it difficult to determine who is ACA full-time and requires an offer of health coverage
- They employ workforces that disproportionately decline offers of health coverage benefits, creating a heavier employer burden in tracking declinations
- Employees come and go during the year with high staff turnover rates, increasing the employer’s burden to track all such employees
- Per diem piece work and multiple rates of pay complicate the determination of pay rates and affordability
- Reliance on payroll systems (or other software programs) that collate data and submit Forms 1094-C and 1095-C often result in a failure to let you know when the data used is inaccurate, which will trigger ACA penalties
Determining the accurate full-time and part-time status of employees under the ACA is arguably the first, and most important, step for ACA compliance. There are real ramifications for inaccurately classifying employees.
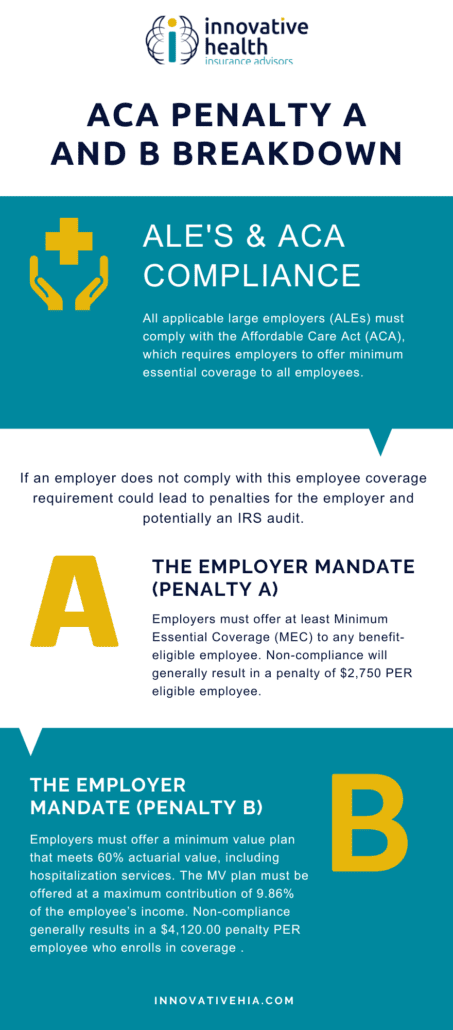
Under the ACA’s Employer Mandate, ALEs, or employers with 50 or more full-time employees and full-time equivalent employees to:
- Offer Minimum Essential Coverage (MEC) to at least 95% of their full-time employees (and their dependents) whereby such coverage meets Minimum Value (MV); and
- Ensure that the coverage for the full-time employee is affordable based on one of the IRS-approved methods for calculating affordability
ALEs that fail to comply with these requirements can be subject to Internal Revenue Code (IRC) Section 4980H penalties.
For example, let’s look at an employer that improperly classifies an employee as not full-time and does not make an offer of insurance. That employee goes to a government marketplace exchange to purchase health insurance and receives a Premium Tax Credit (PTC) that helps subsidize the cost of the health insurance purchased on the exchange. This can trigger the issuance of an IRS Letter 226J penalty notice under IRC 4980H.
The penalty assessment will be applied to every full-time employee working for that employer during the course of the tax year, not just the employee obtaining the PTC. For the 2022 tax year, that penalty could be as high as $275,000 for every 100 employees.
The first step in the full-time status evaluation is determining which measurement method is best for your organization.
For organizations made up primarily of variable-hour employees, you will want to implement the Look-Back Measurement Method. If your workforce has mostly full-time employees and non-varying schedules, the Monthly Measurement Method will be best.
The most expedient step for employers is to get your ACA Vitals score. This will help determine your risk of receiving IRS penalties by analyzing your unique workforce composition.
Such a review can reap dividends by helping employers avoid significant ACA penalties from the IRS, particularly if those organizations have not been filing ACA-required information annually with the IRS. These organizations should file this information as soon as possible to avoid receiving an IRS penalty notice and to minimize potential penalties.
The IRS is currently issuing warning notices to employers identified as having failed to file and furnish Forms 1094-C and 1095-C for the 2019 tax year via Letter 5699. If you have received one, contact us to have the penalty reduced or eliminated. We’ve helped our clients prevent over $1 billion in ACA penalty assessments.
If you are part of the home healthcare, personnel staffing, restaurant and construction industries, or any industry that relies on a significant mix of full-time and part-time employees, you are at serious risk of being penalized for not complying with the ACA.
We see daily how the IRS is enhancing its methods for identifying employers that are not complying with the ACA and sending them penalty notices.
We regularly see the surprise and shock expressed by organizations that receive these penalty notices, many of them containing significant penalty assessments.
We also see how these organizations could have avoided these penalty assessments by receiving help from experts that understand ACA and IRS regulatory requirements and know how to successfully meet those regulatory requirements.