Article originally published on SBMA Benefits.
There are strict deadlines for open enrollment each year. It opens nationally on November 1st and closes on January 15th. Some states, such as New York and California, have extended deadlines through January 31st. Click here to see your state’s open enrollment period.
During this period, people have the opportunity to enroll in healthcare coverage or change their plans. Failing to take action during this time can pose serious consequences because open enrollment is the time employers can take advantage of having health, dental, vision, life, and other voluntary benefit insurance plans. Enrolling after the deadline means that there is no way to make changes to your plan or enroll again until it opens back up a year later.
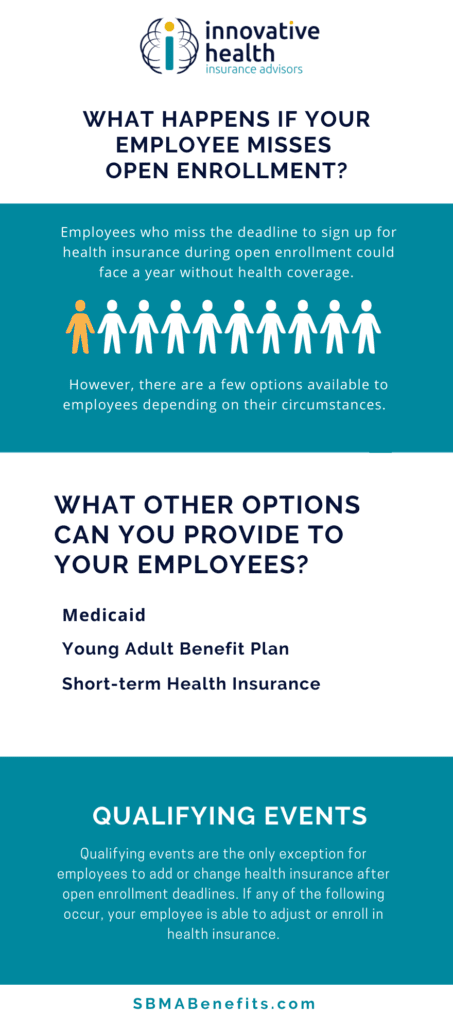
What Happens if Your Employee Misses Open Enrollment?
Employees who miss the deadline to sign up for health insurance during open enrollment could face a year without health insurance. In turn, those without coverage may have to pay an individual mandate penalty on their next tax return. However, there are a few options available to employees depending on their circumstances.
What Other Options Can You Provide to Your Employees?
Depending on the employee’s circumstances, they may be eligible to register for alternative coverage options.
Medicaid
Enrollment for Medicaid is open year-round to those seeing to apply. Eligibility is based on federal requirements that differ depending on the state. It extends coverage for:
- Low-income adults
- Children
- Pregnant women
- Elderly adults
Short-Term Health Insurance
Private insurance companies offer short-term health insurance policies. Most do not cover pre-existing conditions nor do they guarantee coverage because they are not required to fit ACA minimum essential coverage (MEC) benefits.
Young Adult Benefit Plan
Those under 26 years old are eligible to join their parent’s plan if that plan offers dependant coverage. This plan does not require the child to be employed, be a student, or have a child. A caveat may include that registration for the child may need to occur during open registration. Rules and regulations for this may vary depending on plan type and state location.
Qualifying Events
If a qualifying event occurs, employees have the opportunity to change their plans.
Qualifying events are the only exception for employees to add or change health insurance after open enrollment deadlines. If any of the following occur, your employee is able to adjust or enroll in health insurance:
- Marriage
- Divorce if the divorce is counted as a qualifying event by the insurer, or the divorce causes a loss of health coverage
- Death in the family
- Birth of a child
- Adopting a child
- Loss of health coverage
- Turning 26 and losing eligibility as a dependant
- Becoming a United States citizen
- Increased pay that moves the employee out of the Medicaid coverage gap
- Change in income changing eligibility requirements
- Grandfather or grandmother plan renewal
- Moving to an area where there are different health plans
- Changing jobs